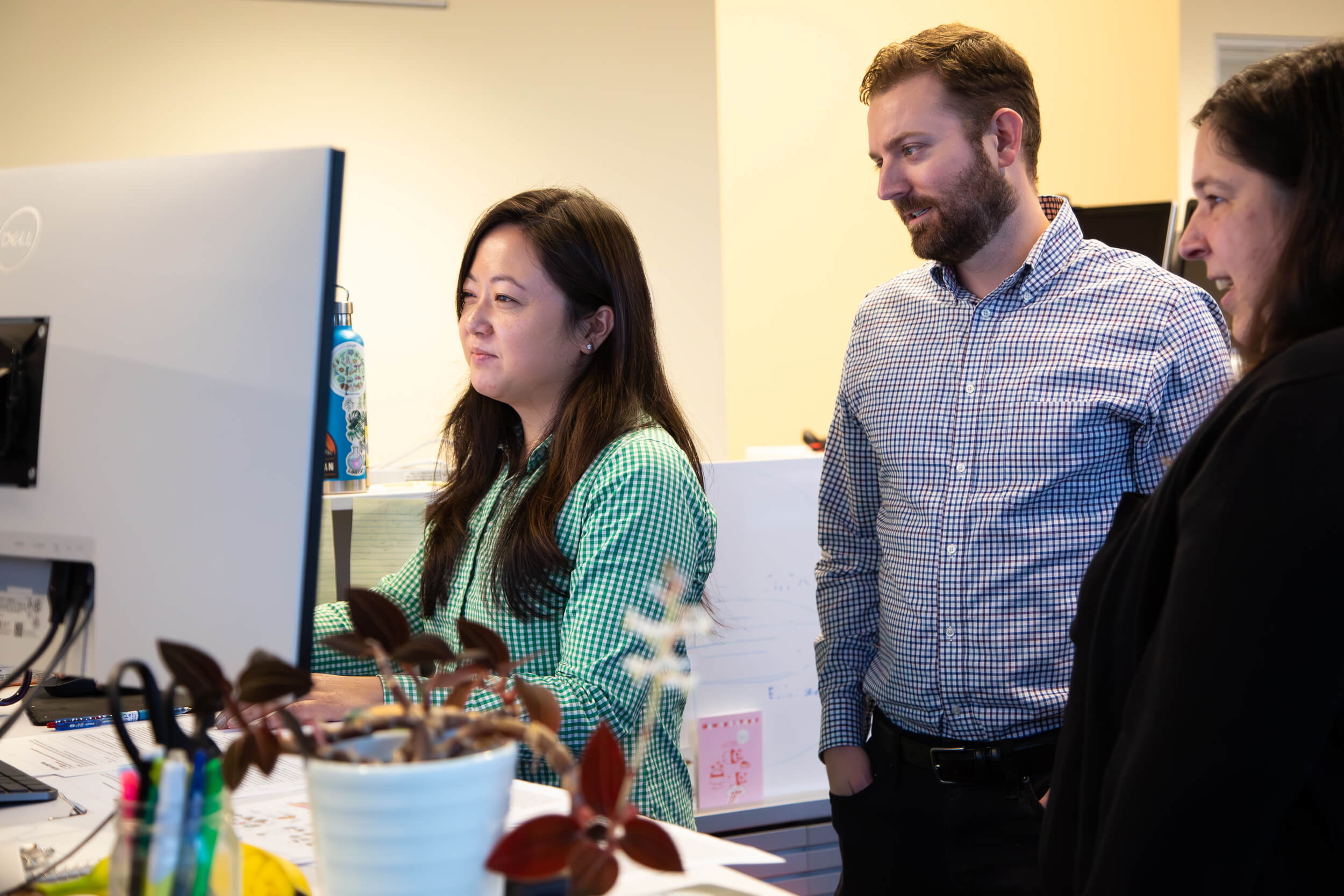
Liz Dueweke / Allen Institute
January 01, 2025
Largest study on brain aging points to possible connections between diet, inflammation, and brain health
Scientists at the Allen Institute have identified specific cell types in the brain of mice that undergo major changes as they age, along with a specific hot spot where many of those changes occur. The discoveries, published in the journal Nature, could pave the way for future therapies to slow or manage the aging process in the brain.
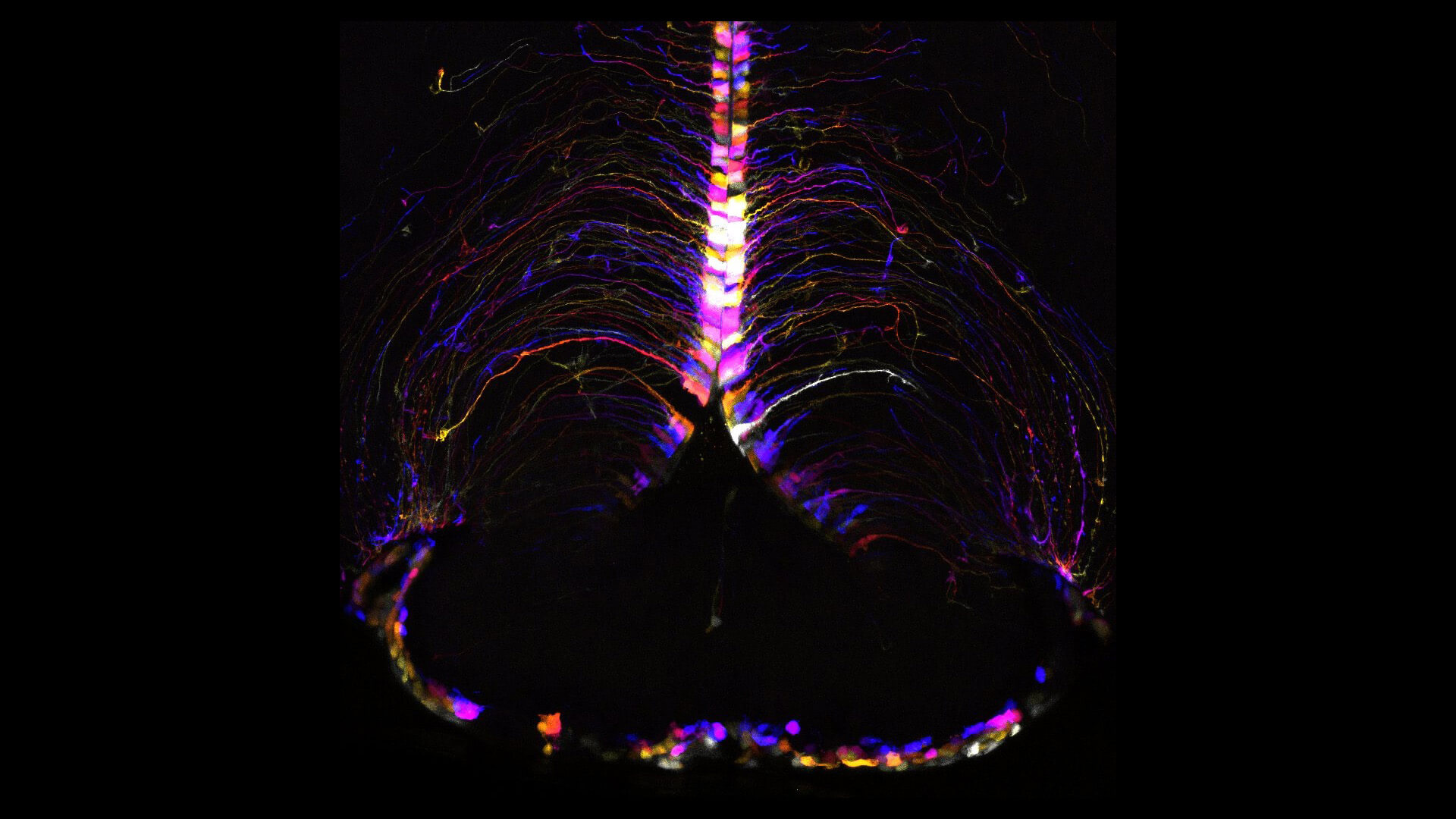
Sensitive cells: Scientists discovered dozens of specific cell types, mostly glial cells, known as brain support cells, that underwent significant gene expression changes with age. Those strongly affected included microglia and border-associated macrophages, oligodendrocytes, tanycytes, and ependymal cells.
Inflammation and neuron protection: In aging brains, genes associated with inflammation increased in activity while those related to neuronal structure and function decreased.
Aging hot spot: Scientists discovered a specific hot spot combining both the decrease in neuronal function and the increase in inflammation in the hypothalamus. The most significant gene expression changes were found in cell types near the third ventricle of the hypothalamus, including tanycytes, ependymal cells, and neurons known for their role in food intake, energy homeostasis, metabolism, and how our bodies use nutrients. This points to a possible connection between diet, lifestyle factors, brain aging, and changes that can influence our susceptibility to age-related brain disorders.
“Our hypothesis is that those cell types are getting less efficient at integrating signals from our environment or from things that we’re consuming and that loss of efficiency somehow contributes to what we know as aging in the rest of our body. I think that’s pretty amazing, and I think it’s remarkable that we’re able to find those very specific changes with the methods that we’re using.”
— Kelly Jin, PhD., scientist at the Allen Institute and lead author of the study
“Aging is the most important risk factor for Alzheimer’s disease and many other devastating brain disorders. These results provide a highly detailed map for which brain cells may be most affected by aging,” said Richard J. Hodes, M.D., director of NIH’s National Institute on Aging. “This new map may fundamentally alter the way scientists think about how aging affects the brain and also provides a guide for developing new treatments for aging-related brain diseases.”
A path toward new therapies
Understanding this hot spot in the hypothalamus makes it a focal point for future study. Along with knowing which cells to specifically target, this could lead to the development of age-related therapeutics, helping to preserve function and prevent neurodegenerative disease.
“We want to develop tools that can target those cell types. If we improve the function of those cells, will we be able to delay the aging process?”
— Hongkui Zeng, Ph.D., executive vice president and director of the Allen Institute for Brain Science

The latest findings also align with past studies that link aging to metabolic changes as well as research suggesting that intermittent fasting, balanced diet, or calorie restriction can influence or perhaps increase life span.
“It’s not something we directly tested in this study,” said Jin. “But to me, it points to the potential players involved in the process, which I think is a huge deal because this is a very specific, rare population of neurons that express very specific genes that people can develop tools for to target and further study.”
Future brain aging research
This study lays the groundwork for new strategies in diet and therapeutic approaches aimed at maintaining brain health into old age, along with more research on the complexities of advanced aging in the brain. As scientists further explore these connections, research may unlock more specific dietary or drug interventions to combat or slow aging on a cellular level.
“The important thing about our study is that we found the key players—the real key players—and the biological substrates for this process,” said Zeng. “Putting the pieces of this puzzle together, you have to find the right players. It’s a beautiful example of why you need to study the brain and the body at this kind of cell type-specific level. Otherwise, changes happening in specific cell types could be averaged out and undetected if you mix different types of cells together.”
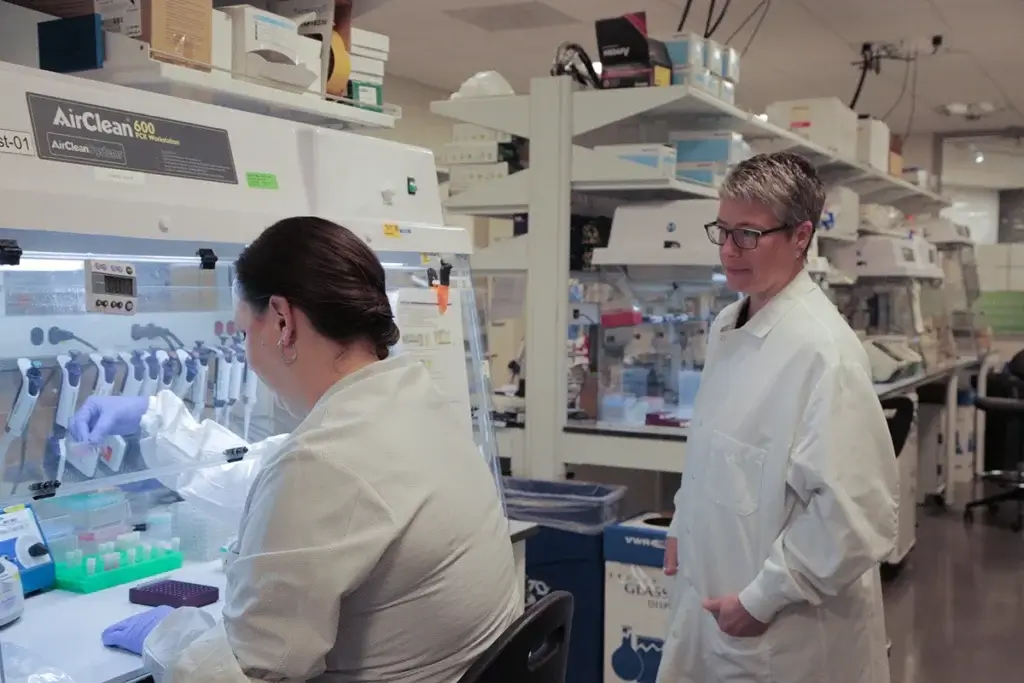
Photo by Jenny Burns / Allen Institute
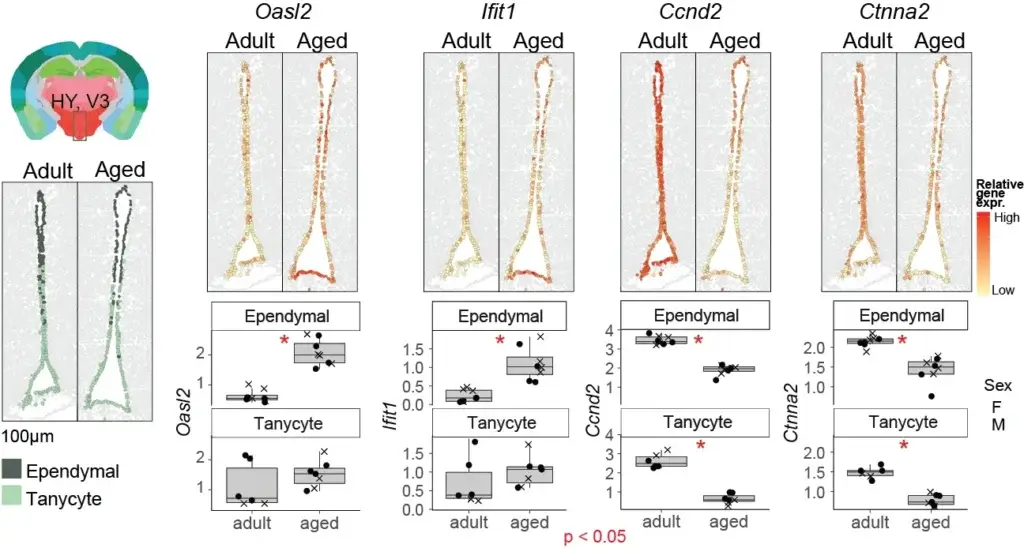

Photo by Jenny Burns / Allen Institute

This study was funded by NIH grants R01AG066027 and U19MH114830. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.

